COVID-19
Two years COVID-19:Looking back and forward
V. Stop the outbreak
The right strategies against a virus are more important than preparedness. The Global health score [GHS], the theoretical preparation of countries against an epidemic correlated negatively with the mortality score due to this epidemic.[JJ] The default responses is minimize infections,[JJ, JJ, JJ, JJ] but some scientists from the UK and the Netherlands advocated mitigation strategies against the outbreak.[Anderson] The WHO advices contact tracing even though it could be challenging for countries to establish a large enough group for this such a system. Military forces could be used to rescue contact tracing.[JJ] Experience and evidence show that when systematically applied, contact tracing can help to break chains of transmission of infection and be a tool for keeping societies open.[WHO]
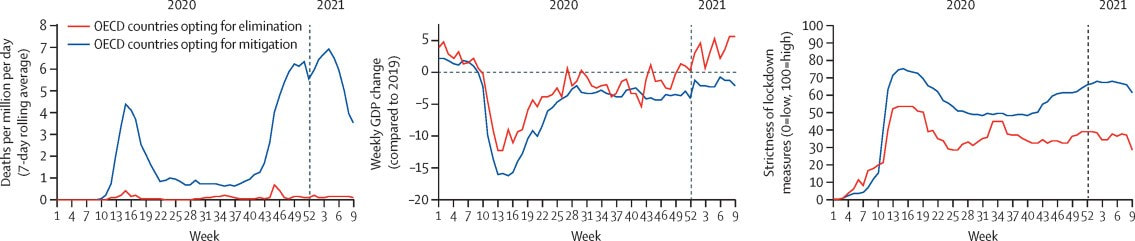
Zero-covid strategies aim to eliminate virus infection by a proactive strategy. Mitigation strategies primarily aim to prevent that health systems are being overwhelmed. Zero-Covid strategies are more effective than mitigation strategies in reducing mortality, limiting economic damage and minimizing impact for society (Figure 1) [Oliu-Barton] Moreover, mitigation strategies bare risks related to virus evolution, persistence, reinfection and causes of disease. It is essential to reduce long-term risks from this incompletely-understood virus and to reduce the risk of the evolution of new variants. [Desforges]
Viruses spread from infected human to uninfected human, thus minimizing infections requires avoiding that infected humans come in close contact with uninfected humans. This method could be split in identifying infected people and isolating these only and isolating everyone in society. It should be repeated that vaccination is of little help in stopping the virus spread.
With everyone So what are the options? The list of options to be discussed:
The best management of hospital capacity is (1) to stop the virus spread by testing, (2) if needed by lockdown, (3) to optimize treatment mainly by vaccination. The latter four strategies are often communicated or even applied, but lack the strive for moral good.[JJ]
Zero-covid strategies aim to eliminate virus infection by a proactive strategy. Mitigation strategies primarily aim to prevent that health systems are being overwhelmed. Zero-Covid strategies are more effective than mitigation strategies in reducing mortality, limiting economic damage and minimizing impact for society (Figure 1) [Oliu-Barton] Moreover, mitigation strategies bare risks related to virus evolution, persistence, reinfection and causes of disease. It is essential to reduce long-term risks from this incompletely-understood virus and to reduce the risk of the evolution of new variants. [Desforges]
Viruses spread from infected human to uninfected human, thus minimizing infections requires avoiding that infected humans come in close contact with uninfected humans. This method could be split in identifying infected people and isolating these only and isolating everyone in society. It should be repeated that vaccination is of little help in stopping the virus spread.
With everyone So what are the options? The list of options to be discussed:
- Quarantine infected people
- Shielding and lockdown
- Optimize (preventive) treatment
- Me first and you not
- Maximize COVID mortality
- Stop our healthcare system
- Repeat mistakes without lessons learned
The best management of hospital capacity is (1) to stop the virus spread by testing, (2) if needed by lockdown, (3) to optimize treatment mainly by vaccination. The latter four strategies are often communicated or even applied, but lack the strive for moral good.[JJ]
Figure 1. Efficacy of elimination (zero-covid) and mitigation strategies with relation to dmortality, GDP loss and duration of lockdown. [Oliu-Barton]
Option 1. Isolate* infected people
The most effective intervention with limited impact on society is to isolate infected people only. Infected people can be identified by testing only, since symptoms develop 1 to 3 days after the highest virus load.[Jones] Testing people on the basis of complaints will miss the most infectious people. Population testing both costs a lot of resources, and is rather ineffective due to the relative high number of false positives when the virus circulates at low frequency in the population. When a test has 0.1% false positives, but only 0.01% of the population has the virus, 91% of the positive test results will be related to uninfected people. This would work if it is much better to be safe than sorrow. In Germany the default policy is that people meeting groups e.g., teachers or care workers, test themselves prior to go working.
A more refined approach of testing is testing people suspected to have been a source or contact of a case i.e., test, trace and isolate (TTI) – the default anti-epidemic strategy.[JJ] As explained before, vaccination has a limited efficacy against infection, and most people with breakthrough infections had high virus load [Begwerk] Not every test has the same reliability and sensitivity and specificity, especially rapid or self-testing for virus antigens might not detect low virus titers.[JJ] But any validated test is much more sensitive and specific than disease symptoms, [RTL] since people will have the highest virus loads one to three days prior to onset of symptoms.[Jones] The ability to screen the most contagious people should not be missed after a potential contact with a contaminated person or when (small) groups of people gather together.
Asymptomatic spreading
Asymptomatic individuals carrying SARS-CoV-2 are hidden drivers of the pandemic, these are crucial but difficult to detect.(see IV) [Gandhi, Long, Boyton Fraser] To stop the epidemic, asymptomatic and presymptomatic infected people should be detected and isolated before they infect others. Waiting for symptoms to occur will be too late to stop most virus spreading.
No infected people, no spreading
Preventive testing is an efficient way to allow small groups to gather together safely.[T, RKI] The strategies to avoid virus spreading are first to inform people when they’re infected to isolate. Contact tracing allows efficient use of sensitive tests.[JJ] Due to false-negative results, no test will offer 100% safety, especially not when virus circulation is high. In those cases additional measures could be taken, like self-testing before meeting in small-sized groups and no meetings of major groups.[JJ] Also lockdown measures could be applied, while balancing safely between risks and precautions, based on actual infection rate within the population.
Testing and quarantine of infected people is an epidemiological measure to protect other people from the virus. It is unrelated to the medical severity of disease. The European GDPR offers a good international ethical framework on privacy-preserving policies for (app) identification needed to verify tested status. Which rules are relevant e.g., vaccinated, cured and tested (see IV), is determined by national health policies. The world lacks the ethical framework and 40 other countries have adapted the European generic concept on privacy protection. In future perspective, these ethical guidelines might be crucial for international healthcare collaboration.
A more refined approach of testing is testing people suspected to have been a source or contact of a case i.e., test, trace and isolate (TTI) – the default anti-epidemic strategy.[JJ] As explained before, vaccination has a limited efficacy against infection, and most people with breakthrough infections had high virus load [Begwerk] Not every test has the same reliability and sensitivity and specificity, especially rapid or self-testing for virus antigens might not detect low virus titers.[JJ] But any validated test is much more sensitive and specific than disease symptoms, [RTL] since people will have the highest virus loads one to three days prior to onset of symptoms.[Jones] The ability to screen the most contagious people should not be missed after a potential contact with a contaminated person or when (small) groups of people gather together.
Asymptomatic spreading
Asymptomatic individuals carrying SARS-CoV-2 are hidden drivers of the pandemic, these are crucial but difficult to detect.(see IV) [Gandhi, Long, Boyton Fraser] To stop the epidemic, asymptomatic and presymptomatic infected people should be detected and isolated before they infect others. Waiting for symptoms to occur will be too late to stop most virus spreading.
No infected people, no spreading
Preventive testing is an efficient way to allow small groups to gather together safely.[T, RKI] The strategies to avoid virus spreading are first to inform people when they’re infected to isolate. Contact tracing allows efficient use of sensitive tests.[JJ] Due to false-negative results, no test will offer 100% safety, especially not when virus circulation is high. In those cases additional measures could be taken, like self-testing before meeting in small-sized groups and no meetings of major groups.[JJ] Also lockdown measures could be applied, while balancing safely between risks and precautions, based on actual infection rate within the population.
Testing and quarantine of infected people is an epidemiological measure to protect other people from the virus. It is unrelated to the medical severity of disease. The European GDPR offers a good international ethical framework on privacy-preserving policies for (app) identification needed to verify tested status. Which rules are relevant e.g., vaccinated, cured and tested (see IV), is determined by national health policies. The world lacks the ethical framework and 40 other countries have adapted the European generic concept on privacy protection. In future perspective, these ethical guidelines might be crucial for international healthcare collaboration.
* In a previous version the text read "quarantine infected people. Although both quarantine and isolation are similar actions, isolation is performed when someone is infected. Quarantine is performed in cases where it is not clear if someone is infected. 06.02.2022.
Option 2. Shielding and lockdown
If testing is insufficient to stop the epidemic, a lockdown might come to rescue. Shielding people might be helpful at moderate virus circulation.
The second effective method against the epidemic would be an generic shielding and lockdown, varying from keeping everyone isolated, to keeping 1.5-2 m distance and wearing masks. These are basically the easy, uninformed albeit limited effective precautions we could take early in the pandemic. Measures could be wearing facemasks, physical distancing, hand hygiene, improving ventilation, filtering air, and avoiding crowded spaces.[WHO] These measures are effective against all flu-like viruses, especially those with low R0 e.g., influenza with R0 ranging from 1.2 to 1.9.[Biggerstaff]
A limited effect of a partial lockdown would help to stop the spreading of the disease by reducing R0 to below 1. In the initial strategy against SARS-2, the Netherlands thought R0 would be 2.2, while I predicted 3.6.[JJ] A week later it seemed to be 3.7, so my estimate was not perfect.[JJ] Importantly with a R0 of 2.2 a partial lockdown e.g., reducing transmission with 50-60% might work to bring R0 to 0.9-1.1, and stabilize the number of infections. However with a R0=3.7, R0 would become 1.5-1.9 still showing strong exponential growth of the number of infections.
Partial lockdown has only limited effect on virus transmission. Sneezing could travel up to 9 meters but doubling the distance from 2 to 4 meters would be related to an 8-fold reduction in virus load. The virus is mostly transmitted through small droplets (aerosols) in exhaled air. A mouth-nose mask might strongly reduce the number of these aerosols.[JJ] Mouth-nose masks do not need to filter the virus out, but filter out the aerosols that carries them. This will be effective too. Breathing through your mask against a mirror will show how much aerosols still are transmitted through the mouth-nose mask. Most masks perfectly filter aerosols from the exhaled air.
These partial lockdown measures, reduce virus transmissions. Recent studies indicate that hand washing, mask wearing and physical distancing, reduce covid incidence by 53%, 53% and 25% in practice.[Talic] Together these measures could aid to reduce the R0 below 1 in the summer, but it might be above 1 in the winter. Prolonged lockdown seriously affects people, [Guedj] and should be minimized. A testing-quarantine procedure is a good alternative to avoid prolonged isolation of people.
The second effective method against the epidemic would be an generic shielding and lockdown, varying from keeping everyone isolated, to keeping 1.5-2 m distance and wearing masks. These are basically the easy, uninformed albeit limited effective precautions we could take early in the pandemic. Measures could be wearing facemasks, physical distancing, hand hygiene, improving ventilation, filtering air, and avoiding crowded spaces.[WHO] These measures are effective against all flu-like viruses, especially those with low R0 e.g., influenza with R0 ranging from 1.2 to 1.9.[Biggerstaff]
A limited effect of a partial lockdown would help to stop the spreading of the disease by reducing R0 to below 1. In the initial strategy against SARS-2, the Netherlands thought R0 would be 2.2, while I predicted 3.6.[JJ] A week later it seemed to be 3.7, so my estimate was not perfect.[JJ] Importantly with a R0 of 2.2 a partial lockdown e.g., reducing transmission with 50-60% might work to bring R0 to 0.9-1.1, and stabilize the number of infections. However with a R0=3.7, R0 would become 1.5-1.9 still showing strong exponential growth of the number of infections.
Partial lockdown has only limited effect on virus transmission. Sneezing could travel up to 9 meters but doubling the distance from 2 to 4 meters would be related to an 8-fold reduction in virus load. The virus is mostly transmitted through small droplets (aerosols) in exhaled air. A mouth-nose mask might strongly reduce the number of these aerosols.[JJ] Mouth-nose masks do not need to filter the virus out, but filter out the aerosols that carries them. This will be effective too. Breathing through your mask against a mirror will show how much aerosols still are transmitted through the mouth-nose mask. Most masks perfectly filter aerosols from the exhaled air.
These partial lockdown measures, reduce virus transmissions. Recent studies indicate that hand washing, mask wearing and physical distancing, reduce covid incidence by 53%, 53% and 25% in practice.[Talic] Together these measures could aid to reduce the R0 below 1 in the summer, but it might be above 1 in the winter. Prolonged lockdown seriously affects people, [Guedj] and should be minimized. A testing-quarantine procedure is a good alternative to avoid prolonged isolation of people.
Option 3. Optimize (preventive) treatment
Vaccination
is the best way to prevent disease. Protection decreases in time but might be
almost 90% during 9 months – the reported efficacies are somewhat higher but
these are measured only in the first 3 months after vaccination. Various
studies suggest that protection by vaccination wanes in time, declines with
age, and even more rapidly wanes in the elderly, indicating that yearly boosts,
preferably just before the winter seasons, are recommended, at least for the
elderly.[Suthar]
The CDC has defined how to calculate protection by vaccination, but the Dutch RIVM uses their own methodology to calculate 95% and 96% protection from hospitalization and ICU admission, respectively. The RIVM model does not correct for time nor waning immunity.[De Gier] In the proper model lower values can be calculated, 85% and 93% protection, respectively.[Smit] It is obvious that misrepresentation of data could have considerable impact on policies,[Westeneng] like revaccination to restore immunity. [BE, IT, IL, FR] Vaccination lowers both cases and deaths, by 6 and 12 fold, respectively.
Besides vaccination, also vitamin D has been shown to personal effect in preventing respiratory diseases, including those of coronaviruses.[Laaksi] Low levels of vitamin D have been associated with severe COVID-19, and restoring vitamin D to normal levels has generic beneficial health effects.[JJ]
The hospital treatment of COVID-19 patients has significantly improved, primarily based on the principles of the virus immune pathology. Generic approaches to reduce inflammation e.g., corticosteroids (dexamethasone) treatment and IL-6 inhibition, are most efficient.[WHO] It should be noted that efficacy of all combined treatments is far less than that of vaccination.
The CDC has defined how to calculate protection by vaccination, but the Dutch RIVM uses their own methodology to calculate 95% and 96% protection from hospitalization and ICU admission, respectively. The RIVM model does not correct for time nor waning immunity.[De Gier] In the proper model lower values can be calculated, 85% and 93% protection, respectively.[Smit] It is obvious that misrepresentation of data could have considerable impact on policies,[Westeneng] like revaccination to restore immunity. [BE, IT, IL, FR] Vaccination lowers both cases and deaths, by 6 and 12 fold, respectively.
Besides vaccination, also vitamin D has been shown to personal effect in preventing respiratory diseases, including those of coronaviruses.[Laaksi] Low levels of vitamin D have been associated with severe COVID-19, and restoring vitamin D to normal levels has generic beneficial health effects.[JJ]
The hospital treatment of COVID-19 patients has significantly improved, primarily based on the principles of the virus immune pathology. Generic approaches to reduce inflammation e.g., corticosteroids (dexamethasone) treatment and IL-6 inhibition, are most efficient.[WHO] It should be noted that efficacy of all combined treatments is far less than that of vaccination.
Option 4. Me first and you not
Not every applied anti-epidemic strategy has high moral values. Not everyone is striving for the common good.[JJ] Two alternative strategies exist (a) to increase the availability of care workers and (b) to reduce the number of patients admitted to the hospital.
I first
Personal protective equipment is essential for care workers e.g., facemasks, that protect both carers and patients. Vaccination does not protect against respiratory virus transmission. The availability of care workers can be increased by vaccinating care workers before high-risk groups. This strategy was rejected on ethical grounds in the EU but the Netherlands employed it anyway.[JJ] This “I first” principle violates the medical ethics that care should be first given to those that need it the most i.e., the risk groups. are required to protect care-workers. Anyone could have an opinion on a captain and crew being the first to leave a sinking ship.
You not
Complementary to “I first” strategy is the “You not” strategy to exclude other people who do not meet your standards. Recently, Austria implemented the 2G-lockdown strategy i.e., only admittance for people who are either vaccinated or cured from SARS-2. This contrasts the countries high availability of testing facilities by mail. Some local authorities practice it in Germany and some main political parties in the Netherlands consider it too. The idea behind this concept is that unvaccinated people would be more likely to be admitted to the hospital. From a technical point of view this is correct but it raises the ethical tension in that it urges people to become vaccinated to retain their freedom. Although it could have beneficial effects e.g., a greater proportion of society might have themselves vaccinated, it also raises the tension in society and decrease the trust in the government and vaccination.[JJ] Trust would be crucial when vaccinations need to be repeated frequently e.g., every year.
I first
Personal protective equipment is essential for care workers e.g., facemasks, that protect both carers and patients. Vaccination does not protect against respiratory virus transmission. The availability of care workers can be increased by vaccinating care workers before high-risk groups. This strategy was rejected on ethical grounds in the EU but the Netherlands employed it anyway.[JJ] This “I first” principle violates the medical ethics that care should be first given to those that need it the most i.e., the risk groups. are required to protect care-workers. Anyone could have an opinion on a captain and crew being the first to leave a sinking ship.
You not
Complementary to “I first” strategy is the “You not” strategy to exclude other people who do not meet your standards. Recently, Austria implemented the 2G-lockdown strategy i.e., only admittance for people who are either vaccinated or cured from SARS-2. This contrasts the countries high availability of testing facilities by mail. Some local authorities practice it in Germany and some main political parties in the Netherlands consider it too. The idea behind this concept is that unvaccinated people would be more likely to be admitted to the hospital. From a technical point of view this is correct but it raises the ethical tension in that it urges people to become vaccinated to retain their freedom. Although it could have beneficial effects e.g., a greater proportion of society might have themselves vaccinated, it also raises the tension in society and decrease the trust in the government and vaccination.[JJ] Trust would be crucial when vaccinations need to be repeated frequently e.g., every year.
Option 5. Maximize COVID mortality
Striving for herd immunity implies maximizing infections, disease cases, long-term impact and mortality. Laymen may be impressed by Van Dissel’s wording “we aim to try to allow a certain amount of infections” and 'titrate' it on the number of hospital admissions and the intensive care unit (ICU) capacity, because "we want to stay below that".[Cloutier] Titration implies to find the maximize the number, in this case to maximize the number of infections that could be handled by hospital admissions and the ICU capacity.
I was utterly surprised to hear this line of reasoning. Maximizing ICU admittance would be considered inappropriate in case of car accidents near schools. Over the last decades we’ve slowed down traffic near most primary schools from 50 km/h to 30 km/h, but with an ICU maximization strategy we could speed up to about 100 km/h near primary schools. I hope this example will highlight the unethical thoughts behind these plans. In an ethical aware society, maximizing disease and mortality rates is unacceptable for any danger, including traffic accidents, cancer, cardiovascular disease and infections. Aiming for zero casualties would always be the desired strategy. Admission to the ICU is not a safe haven, ⅓ to ⅕ people will die at the ICU, not taking in account people who are refused to admission after triage showed they have a poorer prognosis.
Nullifying the value of vaccination
People are admitted to the ICUs because their lives are in danger, and probably about ⅓ or ¼ will die on the ICU. Moreover, if a disease is so severe that some people are admitted to the ICU, others will die before they are admitted to the ICU. Thus basically van Dissel said we want to maximize disease and mortality but not beyond the ICU capacity. In the UK and Sweden similar strategies were followed but not in the rest of Europe.
In the Netherlands ~75% of the whole population is vaccinated[T], and ~ 85% of the adult population.[CD] The mRNA vaccines protect for about 90% against serious disease.#[1] In the wave of spring 2021, ~5% of the population was infected before a lockdown was implemented to stop the epidemic, and avoid a 20-fold higher number. Simple math shows that at least 3 times more unvaccinated could become infected and twice as much as vaccinated people. In total still 5 times higher than the capacity of hospitals and ICUs.[NVIC]
Although vaccination protects individuals from disease, its value would be lost if the policy still aims at maximum capacity of hospitals and ICUs. Because the absolute maximum is higher than the maximum for the hospitals and ICUs, in a vaccinated society the same mortality rate could be achieved by titrating at hospital capacity. A similar concept would be for people dying in car accidents, without or with using safety-belts. If the traffic speed is titrated to the ICU capacity, the safety gain of safety-belts would be lost due to the higher speed as the outcome of the titration. It is not that safety-belts or vaccination are ineffective but titration to the same mortality rates nullifies their efficacies. Paradoxical, the loosened policy could broaden the plateau of maximal casualties, and safety-belts or vaccination would yield more victims due to the underlying evil policies. I’m puzzled to see well-educated people mixing means of anti-epidemic policies with the natural end of an epidemic after failing policies. Or to quote internationally well-respected medical scientist from the World Health Organization (WHO): “Herd immunity is a concept used for vaccination, in which a population can be protected from a certain virus if a threshold of vaccination is reached.” Continuing with “herd immunity is achieved by protecting people from a virus, not by exposing them to it. Never in the history of public health has herd immunity been used as a strategy for responding to an outbreak, let alone a pandemic. It is scientifically and ethically problematic.”
---
[1] I’m aware of higher numbers e.g. 95% in clinical studies with a follow-up of 3 months but immunity wanes in time and vaccination seems to be repeated every 9 to 12 months, not 3 months.
I was utterly surprised to hear this line of reasoning. Maximizing ICU admittance would be considered inappropriate in case of car accidents near schools. Over the last decades we’ve slowed down traffic near most primary schools from 50 km/h to 30 km/h, but with an ICU maximization strategy we could speed up to about 100 km/h near primary schools. I hope this example will highlight the unethical thoughts behind these plans. In an ethical aware society, maximizing disease and mortality rates is unacceptable for any danger, including traffic accidents, cancer, cardiovascular disease and infections. Aiming for zero casualties would always be the desired strategy. Admission to the ICU is not a safe haven, ⅓ to ⅕ people will die at the ICU, not taking in account people who are refused to admission after triage showed they have a poorer prognosis.
Nullifying the value of vaccination
People are admitted to the ICUs because their lives are in danger, and probably about ⅓ or ¼ will die on the ICU. Moreover, if a disease is so severe that some people are admitted to the ICU, others will die before they are admitted to the ICU. Thus basically van Dissel said we want to maximize disease and mortality but not beyond the ICU capacity. In the UK and Sweden similar strategies were followed but not in the rest of Europe.
In the Netherlands ~75% of the whole population is vaccinated[T], and ~ 85% of the adult population.[CD] The mRNA vaccines protect for about 90% against serious disease.#[1] In the wave of spring 2021, ~5% of the population was infected before a lockdown was implemented to stop the epidemic, and avoid a 20-fold higher number. Simple math shows that at least 3 times more unvaccinated could become infected and twice as much as vaccinated people. In total still 5 times higher than the capacity of hospitals and ICUs.[NVIC]
Although vaccination protects individuals from disease, its value would be lost if the policy still aims at maximum capacity of hospitals and ICUs. Because the absolute maximum is higher than the maximum for the hospitals and ICUs, in a vaccinated society the same mortality rate could be achieved by titrating at hospital capacity. A similar concept would be for people dying in car accidents, without or with using safety-belts. If the traffic speed is titrated to the ICU capacity, the safety gain of safety-belts would be lost due to the higher speed as the outcome of the titration. It is not that safety-belts or vaccination are ineffective but titration to the same mortality rates nullifies their efficacies. Paradoxical, the loosened policy could broaden the plateau of maximal casualties, and safety-belts or vaccination would yield more victims due to the underlying evil policies. I’m puzzled to see well-educated people mixing means of anti-epidemic policies with the natural end of an epidemic after failing policies. Or to quote internationally well-respected medical scientist from the World Health Organization (WHO): “Herd immunity is a concept used for vaccination, in which a population can be protected from a certain virus if a threshold of vaccination is reached.” Continuing with “herd immunity is achieved by protecting people from a virus, not by exposing them to it. Never in the history of public health has herd immunity been used as a strategy for responding to an outbreak, let alone a pandemic. It is scientifically and ethically problematic.”
---
[1] I’m aware of higher numbers e.g. 95% in clinical studies with a follow-up of 3 months but immunity wanes in time and vaccination seems to be repeated every 9 to 12 months, not 3 months.
Option 6. Stop our healthcare system
Ignoring COVID-19 would be the most efficient way to eliminate our healthcare system. The alternative foundation Doctors Covid Collective {Stichting Artsen Covid Collectief}, Forum voor Democratie, Willem Engel and Maurice de Hond. I’ve checked but found no relevant, e.g., biomedical, PhDs among these persons and groups. I’ll discuss their strategy since it has a considerable impact on healthcare and society. Although subtle differences exist between these persons and groups, they could all be regarded as opposing options 1 to 5. They reason from limited victims and consider actions to avoid the “Bergamo trauma” as a new and evil religion. [De Hond] The European football match in Bergamo was one of the first steps of the rapid spreading of the virus in Europe, followed by winter sports in the Alps and Carnival in Western Europe.[JJ] In Bergamo there was a 7-fold increase in mortality, which resulted in more than 100.000 COVID-19-related deaths in one year in Italy, 0.2% of the Italian population.[DW]
The Bergamo trauma, however, was that the healthcare system collapsed, and that access to healthcare would be denied for most people based on triage. This prompted Dutch NVIC to write a triage script based on non-medical considerations for ICU admission at the time of phase 3 in the COVID-19 pandemic. Since the spring of 2020, the Netherlands has triage phase 2 over the normal triage phase 1. Normally everyone for which it could be lifesaving is admitted to ICU but in phase 2 only those with the best prognosis and shortest predicted ICU stay. In the phase 3, healthcare is shut down and non-medical grounds determine who will or will not receive medical care. Please note that this is not limited to COVID-19 care but involves all medical care including cardiovascular diseases, cancer, appendicitis and other infections, as well as various other treatable diseases.
Responsible medical doctors fear a healthcare shutdown due to an unmitigated SARS-2 epidemic, and several countries have suffered these due to too late lockdown actions on society. A shut down goes well beyond the impact of maximizing COVID mortality but effectively dismantles our healthcare system. To do nothing against this epidemic would arguably be the worst of all possible options. And for those who only trust on euros, increased revenue from coffin production undermines the economy.
The Bergamo trauma, however, was that the healthcare system collapsed, and that access to healthcare would be denied for most people based on triage. This prompted Dutch NVIC to write a triage script based on non-medical considerations for ICU admission at the time of phase 3 in the COVID-19 pandemic. Since the spring of 2020, the Netherlands has triage phase 2 over the normal triage phase 1. Normally everyone for which it could be lifesaving is admitted to ICU but in phase 2 only those with the best prognosis and shortest predicted ICU stay. In the phase 3, healthcare is shut down and non-medical grounds determine who will or will not receive medical care. Please note that this is not limited to COVID-19 care but involves all medical care including cardiovascular diseases, cancer, appendicitis and other infections, as well as various other treatable diseases.
Responsible medical doctors fear a healthcare shutdown due to an unmitigated SARS-2 epidemic, and several countries have suffered these due to too late lockdown actions on society. A shut down goes well beyond the impact of maximizing COVID mortality but effectively dismantles our healthcare system. To do nothing against this epidemic would arguably be the worst of all possible options. And for those who only trust on euros, increased revenue from coffin production undermines the economy.
Option 7. Repeat mistakes without lessons learned
Progressive insights is the key to progress in science, however many countries still adhere to ineffective early strategies. The UK has not lost its dedication to herd immunity, and still aims for maximizing COVID infections after vaccination. In the Netherlands, independent experts recruited for [Lessons learned] (see above) advised to test and quarantine infected people. Nevertheless the Dutch OMT still opted to maximize COVID mortality, as discussed above. After vaccination, still the balancing-act strategy [Koopmans] is advocated by the thought, unsupported by evidence that people would suffer less at reinfection. The data of common cold shows that repeated infection hardly decrease severity of disease. Basically, this is a renewed attempt to introduce the unscientific and unethical idea of ‘herd immunity’ over virus control.
In theory, I could not rule out that this population-scale experiment with the health of people would work after vaccination, even though it failed before vaccination. However, if the SARS-2 coronavirus behaves like the four well-known human coronaviruses, this strategy will cause a prolonged duration of the epidemic with many more casualties. So far, the data offer no reasons to build on sterilizing immunity, lasting protection from disease, protection against long covid or full protection from disease. With the support of vaccination to reduce the impact of infections, we should still aim for minimizing infections.[JJ]
I predict that repeating the herd strategy after vaccination will cause major hurt for health, economy and society. Vaccination will reduce mortality but not stop the epidemic, with still an overflow for healthcare. To repeat this strategy indicates we failed to learn from reality, as several countries have already shown.
In theory, I could not rule out that this population-scale experiment with the health of people would work after vaccination, even though it failed before vaccination. However, if the SARS-2 coronavirus behaves like the four well-known human coronaviruses, this strategy will cause a prolonged duration of the epidemic with many more casualties. So far, the data offer no reasons to build on sterilizing immunity, lasting protection from disease, protection against long covid or full protection from disease. With the support of vaccination to reduce the impact of infections, we should still aim for minimizing infections.[JJ]
I predict that repeating the herd strategy after vaccination will cause major hurt for health, economy and society. Vaccination will reduce mortality but not stop the epidemic, with still an overflow for healthcare. To repeat this strategy indicates we failed to learn from reality, as several countries have already shown.